Ketogenic diet and insulin resistance
Insulin is a hormone secreted by the endocrine part of the pancreas, namely the beta cells of the islets of Langerhans. It is a very important regulator of carbohydrate metabolism, but also protein and fat metabolism. The main task of insulin is to maintain a constant level of glucose in the bloodstream. When glucose levels rise postmeal, the pancreas releases insulin, which lowers the level of glucose by facilitating its entry into glucose-dependent tissues.
The main roles of insulin include:
- transport of glucose to the liver, adipose tissue and skeletal muscles
- increasing the usage and storage of glucose – increased insulin level activates the processes of glycolysis and gluconeogenesis and inhibits the processes of gluconeogenesis, glycogenolysis and lipolysis
- increasing the use of amino acids for protein synthesis
- increasing fat synthesis by inhibiting lipolysis and beta-oxidation
- inhibition of ketogenesis, ie the oxidation of fatty acids to ketone bodies
- stimulation of the body’s growth and regulation of the action of growth hormone
Glucagon is a hormone counteracting insulin, which is released under the influence of hypoglycemia, i.e. low blood glucose levels. In a healthy person, the insulin level is 10-25 mU/l. Elevated insulin levels are manifested by hunger pangs, hypoglycemic episodes, and weight gain. Symptoms of insulin deficiency include polyuria, weight loss, excessive thirst and non-healing wounds.
Insulin resistance
When muscle, fat and liver cells do not respond properly to the presence of insulin and are unable to properly take up glucose from the blood, it is a state called insulin resistance. As a consequence of persistently high glucose levels, the pancreas secretes more and more insulin to compensate for the poor response of cells to insulin and maintain normal glucose levels.
The pathogenesis of insulin resistance is not yet fully understood, but there are many factors that may increase the risk of its occurrence. In simple terms, insulin resistance is the result of an unhealthy lifestyle, including poor diet and low physical activity. Other factors contributing to insulin resistance include:
- age above 45
- higher cholesterol level
- hypertension
- Polycystic ovary syndrome
- nonalcoholic fatty liver disease
- chronic inflammation
- past gestational diabetes
- previous heart attack or stroke
- a diet rich in sugars and products with a high glycemic index and low in fibre and omega-3 fatty acids
- vitamin D deficiency
- sedentary lifestyle
- certain medications, including corticosteroids and protease inhibitors
- hormonal therapies, including cortisol and growth hormone
- genetic predisposition
Untreated insulin resistance leads to the development of prediabetes and, consequently, diabetes. It should be remembered that prediabetes can also occur without insulin resistance.

Diagnostics of insulin resistance
The diagnostic gold standard for insulin resistance is the euglycemic-hyper insulin clamp method developed by Andres et al. in the 1970s [1]. This method involves the introduction of a constant infusion of insulin to maintain a constant, physiological level of this hormone. At the same time, the glucose level is clamped at the baseline level with glucose infusion at a variable rate to maintain a euglycemic state in the serum (euglycemia – glucose level within normal limits). The amount of glucose uptake is determined per unit of time and is defined by the M value (mmol/kg/min). It is the most reliable and repeatable method, however, it is rarely used in practice due to high costs and the need to perform it in a hospital ward. This method is mainly used in scientific research.
Alternative methods of assessing insulin resistance that can be used routinely include HOMA-IR and the glucose tolerance test.
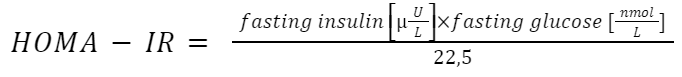
HOMA-IR (Homeostatic Model Assessment of Insulin Resistance) is calculated based on the relationship between insulin and fasting glucose levels. For reliable confirmation of insulin resistance, the HOMA-IR index should be repeated 3-4 times, because fasting insulin levels can fluctuate. A HOMA-IR value greater than 2.5 is considered positive. HOMA-IR is calculated from the formula:
The Oral Glucose Tolerance Test (OGTT) consists of a two-point measurement of glucose level: at fasting and 2 hours after oral administration of 75 g of glucose. It is a method used in diagnosing diabetes, but it can also indirectly inform about insulin resistance.
Treatment of insulin resistance
Treatment of insulin resistance consists in eliminating the factors that primarily contribute to it, i.e. a sedentary lifestyle and a poor diet. Weight loss and lifestyle changes, including increasing physical activity, may improve insulin sensitivity. When insulin resistance is caused by medications or hormonal therapy, a specialist doctor may decide to change the therapy. However, you should not do it on your own!
Ketogenic diet
Since excessive consumption of sugars may contribute to the development of insulin resistance, it seems reasonable to consider whether a diet low in carbohydrates, such as the ketogenic diet, would not be a salutary solution to the problem of insulin sensitivity. Scientific research on carbohydrate metabolism and glycemia has been conducted many times in various study groups.
The results of a meta-analysis (combining the results of many clinical trials to draw more reliable conclusions) from 2020 [2] showed that the use of a ketogenic diet by patients with type II diabetes not only lowered fasting glucose levels (by 1.29 mmol / L), level of glycated haemoglobin HbA1c informing about the metabolic syndrome but also lowered the level of triglycerides, total cholesterol and body weight.
Similarly, a 2023 review [3] that compiled the results of 12 scientific studies conducted on patients with type 2 diabetes and prediabetes reported similar conclusions. Each of these studies showed that the ketogenic diet significantly improved glycemic control. In one of the analyzed studies, despite positive changes in insulin sensitivity, problems with the lipid profile and liver were found. These problems could have been avoided by combining a ketogenic diet with physical activity.
In the case of women struggling with polycystic ovary syndrome (PCOS), in whom increased insulin resistance is very often observed, scientific studies have shown that the use of a ketogenic diet can lower fasting insulin levels and improve hormonal parameters, including testosterone and LH/FSH levels [4].
Similarly, a summary of studies on overweight and obese people showed that the ketogenic diet lowered insulin levels, HOMA-IR and regulated glycemia [5].
The results of the studies and meta-analyses described above unanimously indicate that the ketogenic diet may be a good solution to reduce or prevent insulin resistance. We lack research on the long-term effects of the ketogenic diet, but the knowledge we currently have is very promising. It should be remembered that in the case of people suffering from endocrine diseases (PCOS, diabetes, etc.), the introduction of the ketogenic diet should be carried out under the supervision of a doctor and a dietician.
Bibliography:
[1] DeFronzo R., Tobin J., Andres R.: Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am. J. Physiol. 1979; 237: E214–E223.
[2] Yuan X, Wang J, Yang S, Gao M, Cao L, Li X, Hong D, Tian S, Sun C. Effect of the ketogenic diet on glycemic control, insulin resistance, and lipid metabolism in patients with T2DM: a systematic review and meta-analysis. Nutr Diabetes. 2020 Nov 30;10(1):38. doi: 10.1038/s41387-020-00142-z.
[3] Skow SL, Jha RK. A Ketogenic Diet is Effective in Improving Insulin Sensitivity in Individuals with Type 2 Diabetes. Curr Diabetes Rev. 2023;19(6):e250422203985. doi: 10.2174/1573399818666220425093535.
[4] Mavropoulos, J.C., Yancy, W.S., Hepburn, J. et al. The effects of a low-carbohydrate, ketogenic diet on the polycystic ovary syndrome: A pilot study. Nutr Metab (Lond) 2, 35 (2005). https://doi.org/10.1186/1743-7075-2-35.
[5] Drabińska, N., Wiczkowski, W., Piskuła, M.K. (2021) Recent advances in the application of a ketogenic diet for obesity management. Trends in Food Science & Technology, 110: 28-38. https://doi.org/10.1016/j.tifs.2021.01.080.


